Revenue Management That Secures Your Practice's Full Potential
Retain Maximum Reimbursements, Reduce Administrative Burden
Our behavioral healthcare-specific RCM platform helps you capture every dollar earned while simplifying your billing operations. With enhanced automation, dedicated billing experts, and real-time financial insights, you can focus on patient care while watching your practice thrive financially.


“Incredible software for business insights and efficient automation features"
Simplified Billing, Accelerated Cash Flow,
Patient billing shouldn't consume your time or drain your energy. Opus RCM delivers a powerful, automated solution that ensures every claim gets paid quickly and completely. From initial verification to final payment, we handle the financial details so you can concentrate on clinical excellence and practice growth.
Revenue Cycle Management Services Turn Billing Challenges Into Revenue Opportunities
Convert Denials Into Revenue
Our claim scrubber catches errors before submission, preventing rejections and accelerating payments directly to your bank account.
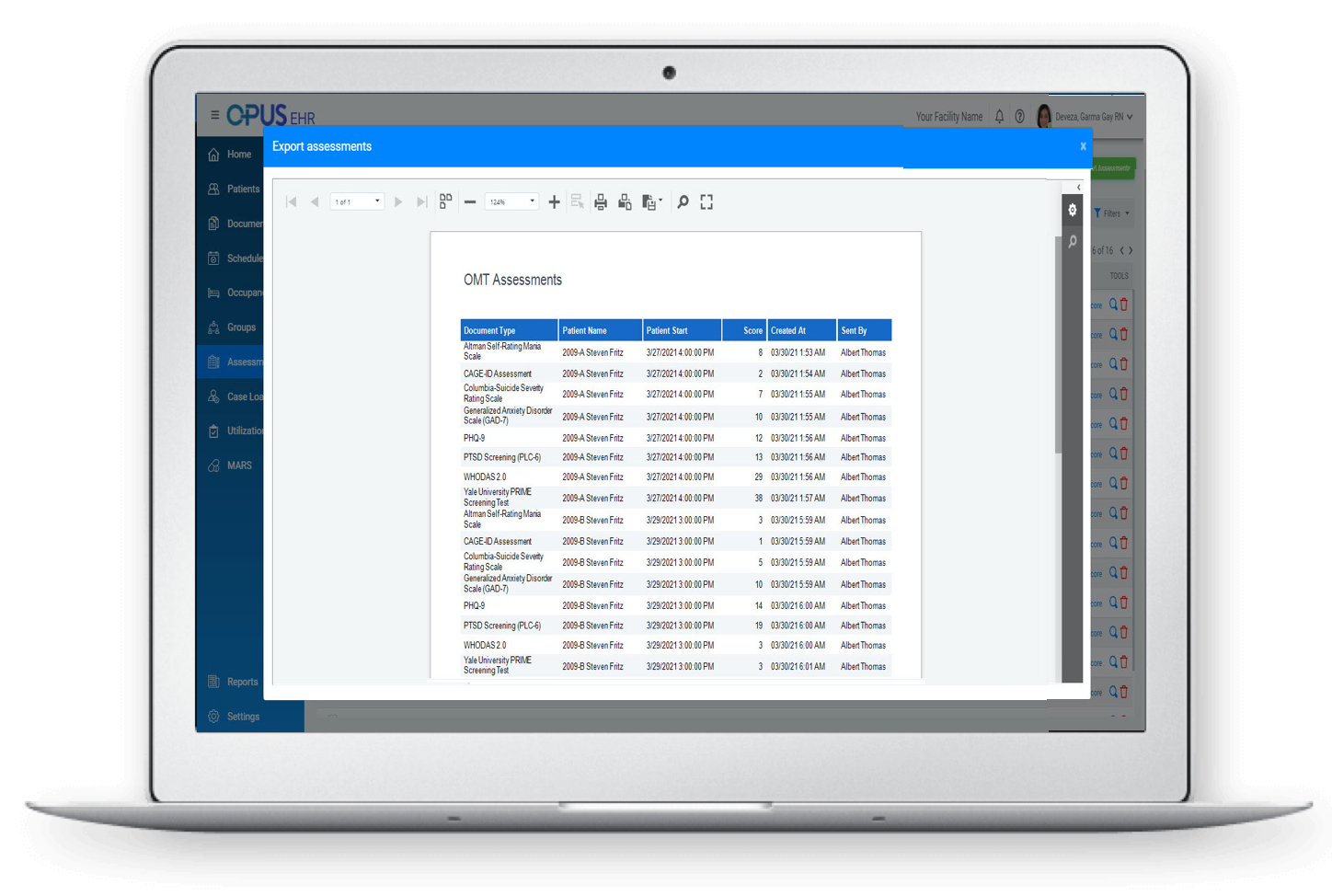
Real-Time Financial Intelligence Dashboard
With intuitive dashboards, you can view critical metrics at a glance, showing exactly where your money stands across all payers and claims.
Complete Revenue Cycle Control - Securing Your Financial Future in Healthcare
RCM isn't just a back-office function—it's the financial heartbeat of your practice. Our comprehensive platform combines cutting-edge technology with healthcare billing expertise to create predictable cash flow. We protect your revenue from claim denials, identify reimbursement opportunities, and build the financial stability you need to invest in your practice's future with complete confidence.
Meet With Opus Team
Let us show you why Opus is right for you. During your meeting, you'll see the Opus workflow in action. We'll guide you through the platform, share information on tools that will help you manage your practice, and answer all of your questions.
Speak with our team today
.png?width=384&height=383&name=image%20(5).png)
Meet With Opus Team
Let us show you why Opus is right for you. During your meeting, you'll see the Opus workflow in action. We'll guide you through the platform, share information on tools that will help you manage your practice, and answer all of your questions.
Speak with our team today
.png?width=384&height=383&name=image%20(5).png)
Meet With Opus Team
Let us show you why Opus is right for you. During your meeting, you'll see the Opus workflow in action. We'll guide you through the platform, share information on tools that will help you manage your practice, and answer all of your questions.
Speak with our team today
.png?width=384&height=383&name=image%20(5).png)
Meet With Opus Team
Let us show you why Opus is right for you. During your meeting, you'll see the Opus workflow in action. We'll guide you through the platform, share information on tools that will help you manage your practice, and answer all of your questions.
Speak with our team today
.png?width=384&height=383&name=image%20(5).png)
TRUSTED BY 160,000+ PRACTITIONERS EVERY DAY
Partnered with the biggest names in the industry



























Why Choose Opus RCM

An RCM Platform Built for Healthcare Professionals
Contrary to general billing systems, Opus RCM understands the nuances of healthcare reimbursement. We've designed our platform to handle the unique complexities of medical billing, from insurance verification to payer-specific claim requirements. Our healthcare-specific tools eliminate the frustration of adapting generic financial software to your specialized needs.
Your All-Inclusive Revenue Management Suite
Automated Claim Processing
Prevents denials automatically for faster, more reliable payments.
Seamless Integration
Works effortlessly with your existing clinical systems.
Full Compliance Support
Shields your practice from penalties and regulatory issues.
User-Friendly Interface
Reveals your financial health at a glance without complexity.
Ready to Renew Your Revenue Cycle?
Take control of your practice finances with Opus RCM. Our team of healthcare billing experts will show you how our platform can reduce your administrative burden while maximizing your reimbursements. Schedule your personalized demo today and discover the difference complete revenue cycle management services can make for your practice.
See What Our Clients Say
After switching to Opus RCM, our collections increased by 23% while our staff spent 40% less time on billing tasks. The system catches billing errors we would have missed, and the financial dashboards give me confidence in our practice finances I never had before.
The Opus team feels like an extension of our practice. They understand behavioral health billing challenges and have helped us easily navigate complex payer requirements. Our days in A/R have decreased dramatically, and we finally have predictable cash flow.
We were drowning in denied claims and spending hours on billing calls before implementing Opus RCM. Within three months, our clean claim rate jumped to 96%, and reimbursements accelerated by weeks. Now I can predict our monthly revenue with remarkable accuracy.